Reports in the All Payer Population Reports mostly contain claims data from the Maryland All Payer Case Mix dataset. However, some reports listed here may combine multiple datasets like Medicaid and Medicare information.
You can learn more about the claims data available to CRISP on this webpage.
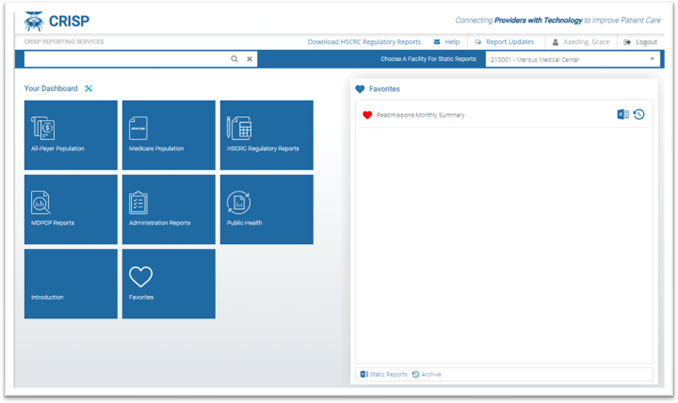
Below are the reports available to users within the All Payer Population Reports category (note: access to these reports is dependent on organization type and HIPAA status):
The Maryland Health Services Cost Review Commission (HSCRC) runs several quality-based measurement and payment initiatives. These initiatives are important policy tools for providing strong incentives for hospitals to improve their quality performance over time. These initiatives hold a portion of hospital revenue at-risk directly related to specified performance benchmarks.
The HSCRC currently runs a series of quality initiatives to ensure that hospitals improve quality in line with targets set in the Maryland All-Payer Model agreement with the Center for Medicare and Medicaid Innovation (CMMI), which runs from 2014-2018. Quality programs provide financial incentives for hospitals to improve or maintain high quality performance on selected quality of care measures. Quality measures are typically classified into three categories: structural (such as patient to provider ratios or use of electronic health records), process (such as percentage of patients receiving preventive services), and outcome (for example, rate of complications). Where possible, the HSCRC works to employ the use of outcome measures. To learn more about the HSCRC Quality programs visit the HSCRC website, register to watch the a full webinar recording, or view this webinar slide deck.
The HSCRC and CRISP produce monthly or quarterly regulatory reports to monitor hospitals based on the HSCRC quality programs. To learn more about these reports click one of the links from Available HSCRC Regulatory Reports below.
Below are the reports available to users within the HSCRC Regulatory Reports category (note: access to these reports is dependent on organization type and HIPAA status):
- Quality Financial Impact Dashboard
- Maryland Hospital Acquired Conditions (MHAC)
- Potentially Avoidable Utilization (PAU)
- Quality Based Reimbursement (QBR)
- Readmissions
- Hospital Population Health Programs – Hospital Inpatient Diabetes Screening
- CDS-A Reports
- Demographic Adjustment
- Market Shift
Reports for the Medicare population based on the Claim and Claim Line Feed (CCLF) data. This includes the MPA reports and the MADE application.
Claim and Claim Line Feed (CCLF): The CCLF (Claim and Claim Line Feed) data files are a set of Medicare claims files incorporating all Medicare Part A and B claims from Inpatient Facility, Outpatient Facility, Skilled Nursing Facility, Home Health Agency, Hospice, Professional, Durable Medical Equipment, and Prescription Drug services. These files contain beneficiary claim level data including Medicare payment amounts, diagnoses, procedures, dates of service, provider identifiers, and beneficiary copayment amounts.
You can learn more about the claims data available to CRISP on this webpage.
Below are the reports available to users within the Medicare Reports category (note: access to these reports is dependent on organization type and HIPAA status):
- Medicare Analytics and Data Engine (MADE)
- Care Transformation Initiative (CTI) and Care Transformation Profiler (CTP)
- MPA Monitoring Reports
- MPA Attribution Tracking Tool (MATT)
- ECIP
- Episode Quality Improvement Program (EQIP)
- Maryland Primary Care Program (MDPCP) Reporting Suite
- Value Based Care Insights (VBCI) Tool
Public health reports contain the reports to support Statewide Public Health Programs, Monitoring, and Research.
Below are the reports available to users within the Public Health Reports category (note: access to these reports is dependent on organization type and HIPAA status):