View Topics & Resources
Explore Topics
Other Resources
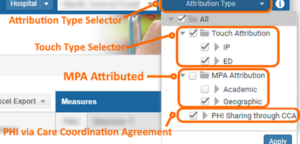
MADE: Attribution Type Selection
HSCRC has a data sharing policy that enables users to view PHI for select beneficiaries with whom they have a treatment relationship (Refer to the MADE PHI Data Sharing Policy Page for more information). MADE contains a drop-down selector that allows users to limit their population to a subset of interest.
In the following sections, we outline how to use the Attribution Type drop-down selector and Patient Navigator columns to select a sub-population of interest based on touch, MPA attribution, and presence of a Care Coordination Agreement (CCA). All attribution types using the drop-down selector in MADE are applied according to OR logic, such that beneficiaries with any of the selected attribution types are included in a user’s current view.
Touch Attribution
Under HSCRC data sharing policies, hospitals are allowed to access PHI for beneficiaries who had an inpatient hospitalization (IP) or emergency department visits (ED) with the attributed hospital in the 36 months of claims data available in MADE. This includes all beneficiaries, regardless of state or county of residence and MPA attribution.
Within Population Navigator, users can identify these beneficiaries using either the Attribution drop-down or the “Touch Attribution Type” column.
Drop-down:
By default, IP touch is selected. Add beneficiaries with an ED touch by checking the box, and clicking Apply. Note that any beneficiaries with both an IP and ED touch are presented with either the single selection of Touch attribution type as well as with both IP and ED selected.
Population Navigator Column:
The “Touch Attribution Type” Column identifies the type of touch that enabled the beneficiary’s PHI to be available to the hospital:
- IP – inpatient admission only
- ED – emergency department visit only
- Both – inpatient admission and emergency department visit
MPA Attribution
Users can filter their MADE population by the two categories of MPA attribution.
Geographic: Beneficiaries are attributed by residing in the hospital’s Primary Service Area (PSA) (or by the PSA Plus (PSAP) methodology). As PSA’s overlap for multiple hospitals, beneficiaries may be attributed to more than one hospital. This attribution does not necessitate a treatment relationship, and therefore hospitals do not have access to beneficiary PHI simply due to MPA attribution.
Academic – Beneficiaries are attributed to an academic medical center (AMC) – either Johns Hopkins Hospital or University of Maryland Medical Center – if they have an inpatient admission with a case mix index (CMI) ≥ 1.5 at the AMC. Academic attribution is agnostic to the beneficiary’s residence or geographically-attributed hospital. By definition, all academically attributed beneficiaries are presented in MADE, as the IP touch criteria has been met.
Geographic and Academic attribution is not mutually exclusive; therefore, beneficiaries can be attributed to the same – or to different – hospitals simultaneously under these approaches.
Drop down:
Select the available MPA Attribution option(s) to load all available beneficiaries MPA attributed to the hospital.
Population Navigator Column:
The “MPA Attribution” column indicates whether and under which approach a beneficiary is MPA Attributed to the hospital.
- Geographic – Geographically attributed only under MPA
- Academic – Academically attributed only under MPA
- Both – Geographically and academically attributed under MPA
PHI Sharing through CCA
Hospitals may attest to legal arrangements with providers (individual clinicians and facilities). Through these arrangements, hospitals are allowed to view PHI-level data for beneficiaries with treatment relationships with those providers. These arrangements – referred to as Care Coordination Agreements (CCAs) – can include employment contracts and other official arrangements. A treatment relationship is defined differently for clinician and facility partners:
- Clinician partners: The beneficiary has at least one claim from the clinical partner within the last 36 months in which an Evaluation and Management (E&M) procedure code was billed.
- Facility partners: Each beneficiary that has an admission/episode of care within the last 36 months from the facility partner.
PHI Sharing through CCA allows beneficiary PHI level data to be shared with hospitals.
Population Navigator Columns: There are two, non-mutually exclusive columns corresponding to PHI Sharing through CCA with Yes or No values indicating the presence or lack thereof of a treatment relationship. Note that in many cases, the presence of the CCA is the mechanism that allowed the PHI to be shared with the hospital (except for when a Touch is also present).
- “Treated by Clinician in CTO”
- Maryland Primary Care Program (MDPCP) providers in the hospital-based Care Transformation Organization (CTO) with whom a beneficiary has had a qualifying E&M visit.
- “Treated by Clinician/Facility with CCA”
- Clinician or facility with legal arrangement outside of either MDPCP relationship above as attested by the hospital.

